Mylo was diagnosed just before he was a year old. Our health visitor was concerned about his fat tummy and he’d stopped growing. We were soon on a roller coaster of blood tests, liver biopsy, scans, finger-pricks, physiotherapy and a feeding regimen. Our local hospital, East Surrey, transferred Mylo to Kings College London before finally he was admitted to the Evelina Children’s Hospital, London.
Learning the routine for regular feeds
We experienced a mixture of emotions during our two-week stay at Evelina; being trained to insert a nasogastric (NG) tube, to feed through the tube and to replace it when it comes out. We had to feed Mylo every three hours, on time, including night-time feeds. Children with GSD3 cannot be fed ten minutes late, otherwise blood-sugar levels drop rapidly!
As Mylo must eat often, he never feels hungry so picks at food. Always clock watching is one of the hardest parts of living with this condition. Mylo can’t fit in with us, we must adjust around him, simple things like when travelling – pulling over to feed him.
We never really had time to think about what this condition would mean for us as a family, or Mylo, long-term. One thought was “Can we still go camping?” – the answer is “Yes”, but we must take copious supplies on a fortnight’s holiday. We have to triple-check all items delivered to our home, as they can’t be purchased from a local chemist should we run out.

Regular visits to the Evelina.
Regular visits to the Evelina for checks
All trust is in the NHS; the wonderful doctors, consultants and nurses who treated our son made us realise just how ill he’d been in his first year. Mylo even spent his first birthday in hospital, having been taken from his party by ambulance after his body couldn’t cope with the immunisations of the previous day.
We visit the Evelina multiple times each year and Mylo spends two days in hospital for his profile assessment each year. This is to ensure his feeding regime is on schedule, or whether it should be tweaked as he grows. Mylo never really complains; apart from having a cannula inserted regularly, and his PEG changed every 3-6 months. GSD3a means that Mylo’s heart is affected and he must have a regular electrocardiogram (ECG). It’s a condition for life, which he must learn to live with.
Mylo is now regularly fed through his Percutaneous Endoscopic Gastrostomy (PEG) so never feels hungry and doesn’t often eat orally. This is improving as he grows, but he’s still a long way from eating a normal dinner. The hardest time is when his treatment falters; to be woken at night by his screaming out in agony during a fit due to hypoglycaemia. We quickly administer emergency treatment before calling 999. Then, on the way to A&E, try to hold ourselves together whilst comforting our daughter.

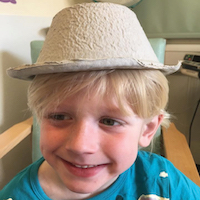
Just an ordinary boy, with a big smile.
We never treat him differently
Mylo attends a mainstream school and has three one-to-one teaching assistants. GSD3a affects all muscles so Mylo’s fine motor skills suffer; he has weak fingers and struggles with buttons, zips, handwriting and anything fiddly. He uses a writing slope to prevent scrunching of his shoulder blades and uses a finger grip to write and a footrest for support.
Gross motor skills are also affected, he struggles with running, stairs, walking any distance, and relies on a disability pushchair. He can’t ride a bike yet, unlike his friends. Mylo struggles to keep up with his peers at school, Cub Scouts and swimming, but always tries. We have never treated him differently; he’s just an ordinary boy whose body doesn’t function normally.